Proton radiotherapy differs from photon radiotherapy by the absorption of ionizing radiation in the tissues. In general, proton radiotherapy has a better dose distribution in the area of medium and low doses of radiation and similar dose distribution in the area of high doses. Low and medium doses are source of late and very late side effects of radiotherapy, and therefore its use should be considered especially in situations where long survival of the patient is expected. Protons are also beneficial for tumors located near healthy tissues, which can be damaged by radiation in the short-term, where photon radiotherapy does not allow the administration of doses sufficient to eradicate the tumor.
Indications for proton radiotherapy at PTC reflect international recommendations (such as ASTRO Proton Beam Therapy Model Policy, latest update 2017), as well as indications used in other proton centers. An example is a summary published by authors from the USA associated with the Pediatric Proton Consortium Registry, or a publication describing the indications used in 40 proton centers, not only in the USA, but also in Europe and other continents, in which PTC also participated.
Target volumes, fractionation and the timing of radiotherapy for individual subgroups of pediatric tumors are specified in the respective pediatric protocols. The rule is that the fractionation, volume and dose are the same as in the case of photon radiation therapy. The advantage of proton therapy is the achievement of greater conformity with the lower integral dose. Unlike adult patients, it can be generalized, that accelerated radiotherapy regimens are not used in pediatric patients and normal fractionation is the standard of treatment.
Advantages of Proton Therapy
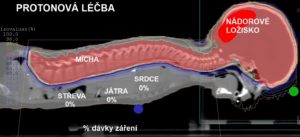
Proton radiotherapy is associated with the sparing of the tissue “in front of the tumor” (from the perspective of the radiation source) and in particular beyond the tumor. In this way, it is possible to deliver the prescribed dose to the target volume while sparing the healthy tissue (as compared to photon radiation), improve the toxicity, and improve the quality of life of pediatric patients. In particular, it is thought that the percentage of tumors induced by irradiation after proton radiotherapy will drop significantly, since the percentage of irradiated healthy tissue decreases considerably in comparison with photon therapy.

Purchase the book via the link below.
Purchase the book via the link below.