
Determining a target volume during irradiation of the esophagus is based on several specifics:
For these reasons, the target volume in radical radiotherapy should include:
Elective irradiation of lymphatics is a circumstance at the center of attention when irradiating esophageal tumors. In clinical studies, which demonstrated the efficacy of radiochemotherapy, various areas were included in the elective irradiation of lymphatics. According to the current consensus, it is beneficial to include in the target volume all the areas with a risk higher than 15-20%. The risks of lymph node involvement, depending on the site of the primary tumor in the esophagus, has been described in several studies based on lymphadenectomy findings. Marked differences are seen in the quantification of risks. The reported differences suggest some uncertainty in risk classification and the non-homogeneity of clinical trials with respect to study groups, which included mostly squamous-cell carcinoma. In contrast, no clear differences have been demonstrated between adenocarcinoma and squamous-cell carcinoma in the risk of lymphatic area involvement.
The distribution of risks, according to the sections of esophageal involvement in the largest referenced group, is schematically shown in Figure 1. The distribution of risks shows how large the volume of elective irradiation of lymphatics requires at risk above 15%. In general, the rule of including two adjacent floors in the irradiated volume can also be applied. For example, for tumors of the middle thoracic region, a large nodal area from the cervical to the upper abdominal nodes will be included in the volume.
Figure 1: Risk of involvement of nodal areas depending on the primary location of the tumor.
Application of proton irradiation in consensual protocol therapy of tumors of the esophagus has been tested at several sites in the world, especially in Japan and USA. Published data include dozens of treated patients. Ie. publications are phase II trials, rarely at the level of phase III studies.
You can derive some conclusions:
Figure 2: Example of an irradiation plan and dose distribution to individual organs. It is clear that a significantly lower or zero dose is applied to healthy tissues during proton radiotherapy.
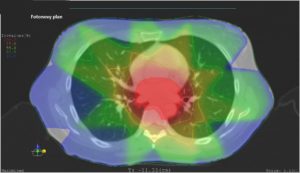
Photon Plan
Proton Plan
The proximity of radiosensitive organs such as lungs, heart, spinal cord, liver, kidneys and potentially thyroid gland and a complex geometric shape of the irradiated volume, markedly complicate the achievement of an effective therapeutic range. The risks of late adverse effects that may result in failure of the respective organs are of vital importance. Limited integral dose or maximum dose to the respective organs (“dose constraints”) are listed in the following table:
Table 1: Obligatory “dose constraints” for irradiation of esophageal tumors.
| Organ | Maximum integral dose determined by volume of the irradiated organ | Maximum integral dose to the organ determined by its level |
| Lungs | V20Gy < 37% | Dmean < 20 Gy |
| Heart | V33Gy < 60% | |
| Spinal cord | V5% < 50 Gy | |
| Liver | Dmean < 23 Gy | |
| Kidneys | Dmedian < 17 Gy | |
| Esophagus outside the irradiated volume | Entire circumference below 60 Gy |
Limitations of Current Radiation Therapy – Technical and Biological Aspects
Standard preoperative irradiation of a localized esophageal cancer up to a total dose of 50 Gy in 25 fractions, including elective irradiation of lymphatics at 15% risk by photon therapy is difficult and requires the IMRT technique. The geometric shape of the irradiated volume is complex and includes multiple concavities. Even with the use of IMRT, it is difficult to adhere to the dose constraints specified in the above table. When increasing the dose up to a total of 70 Gy to the area of confirmed involvement (outside the volumes of elective irradiation), the difficulty is much higher even when using the IMRT technique.
Radiochemotherapy of esophageal cancer usually has acute and late side effects. The severity of both increases depending on the preoperative approach. The timing of surgery 4 to 6 weeks after the end of radiochemotherapy provides a short time window for the resolution of acute side effects. The risk is a delay of the procedure or permanent inability to undergo the resection procedure. Certain procedures, including thoracotomy and mediastinal lymphadenectomy, are associated with postoperative requirements as to the cardiorespiratory capacity, which may be impaired by the development of chronic toxic effects, with maximum impairment in the postoperative period. When using standard techniques of photon radiotherapy (IMRT, 3DCRT), the risk of any complications is up to 75%.
The risk of chronic adverse reactions in particular is clearly related to the adherence to the aforementioned “dose constraints”. Considering the increasing risks, various limiting integral doses can be defined for the respective organs.
Table 2: Structure for individual dose/organs.
| IMRT (photons) | IMPT (protons) | |
| Target volume (tumor of the esophagus) | 50 Gy (100%) | 50 Gy (100%) |
| Lung (Dmean) | 20,7 Gy (41%) | 2,99 Gy (5,9%) |
| Spinal cord (Dmax) | 47,4 Gy (94%) | 33,0 Gy (66%) |
| Heart (Dmean) | 29,9 Gy (59,8%) | 18,42 Gy (26%) |
| Liver (Dmean) | 21.4 Gy (42%) | 2,38 Gy (4.7%) |
Purchase the book via the link below.
Purchase the book via the link below.