
Concomitant chemoradiotherapy is a standard modality of anal cancer treatment. The disease has
a high cure rate, thanks to the combination of a large volume irradiated, concomitant chemotherapy and the total dose of radiation. However, the risk of early and late side effects is high. More than one third of patients develop acute toxicity of grade 3 or 4.
Currently, patients with carcinoma of the anus are treated with the IMRT technique. A disadvantage of this technique still consists in a high burden to the skin and subcutaneous tissues, the bladder, rectosigmoid colon and loops of the small intestine. Another disadvantage is the high integral dose of radiation delivered using this technique. This results in a high degree of acute toxicity of the treatment, especially acute skin reactions, acute gastrointestinal and genitourinary toxicity, and also hematologic toxicity due to the effects of concomitant chemotherapy. Late side effects are related mainly to fibrotisation of the perianal region, groins and other adjacent tissues. It involves dysfunction of the pelvic floor and sphincters, vaginal stenosis, deformation and dysfunction of external genitalia and obstruction in the groin area.
Treatment of anal tumors has been gradually introduced in proton centers worldwide. The reason is the chance to reduce the integral dose in the entire pelvic area, i.e. the radiation burden to the skin, subcutaneous tissues, bladder, genitalia, rectosigmoid colon and small intestine. Dosimetry studies have been published. The possibility of reducing toxicity is significant especially in those constellations where the toxicity is a long-term limitation, and where the development of IMRT photon radiotherapy techniques brought only a minor improvement and in some cases even an increase in the integral dose as compared to the previous 3 DCRT techniques.
Strategy in Radiation Therapy:
Anal tumors are treated with irradiation of 2 volumes using the SIB technique (simultaneous integrated boost) at 2 dose levels:
The requirements for dose distribution with this technique and the geometric constellation can be optimally managed during proton radiation dosimetry. It offers a significant reduction of doses to the critical structures of the pelvis. This includes mainly reduction of doses to the following structures:
Figure 1: Example of irradiation plan and dose distribution in the pelvis during proton and photon irradiation. It is clear that a significantly lower or zero dose is applied to healthy tissue during proton radiotherapy.
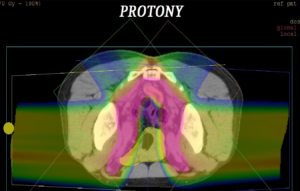
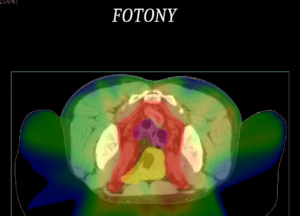
Table 1: Specification of doses to the individual structures/organs.
| Organs at risk | Dose specification | IMPT dose (Gy) | IMRT dose (Gy) |
| Urinary bladder | Dmean | 13,95 | 37,00 |
| Small intestine | Dmean | 8,55 | 26,24 |
| Bulb of penis | Dmean | 22,92 | 44,39 |
| Dmax | 55,52 | 53,54 | |
| Sigmoid colon | Dmean | 18,47 | 38,68 |
| Rectum | Dmean | 44,00 | 43,16 |
| Dmax | 54,84 | 54,60 | |
| Bone marrow in the area of pelvis, sacrum and proximal thirds of the femur. | Dmean | 18,00 |
>35
|
In the patients that have been treated so far at PTC Prague, we observed the following advantages compared to our own experience with photon radiation:
Purchase the book via the link below.
Purchase the book via the link below.