
Pancreatic tumors are treated at proton centers around the world. The reason is a close proximity of critical organs and the tumor that usually does not allow the administration of sufficient doses in photon techniques while respecting the tolerated doses to critical organs. In addition to increasing local control of the disease, the goal is to reduce the long-term adverse effects and improve the quality of life of the patients.
Pancreatic tumors have a poor prognosis. However, they say nothing about the survival length of the patients and about any possibility of influencing the course of the disease. The possibilities have been expanding. In addition, the group of pancreatic tumors is not homogenous at all. About 5% of pancreatic tumors are constituted of neuroendocrine tumours (NET) with much better prognosis. They require completely different treatments. The majority group of epithelial tumors of the exocrine pancreas also includes less common forms classified in the group of cystic and mucinous tumors of the pancreas. These also have a better prognosis and some are even benign. The questions on the use of radiation therapy do not apply to the NET or cystic tumors.
Surgery has always had a fundamental role in the treatment of localized stages of pancreatic carcinoma – total or partial pancreatectomy. In the cancers of the head of the pancreas, which are the most common ones, duodenectomy is used with the restoration of the continuity of anastomoses (hepatojejuno-, gastrojejuno-, possibly pancreatojejuno- or pancreatogastroanastomosis). Only radical resection is beneficial. R1 and R2 type resections lead to an early disease relapse and have minimal impact on the length of survival.
Clinical studies conducted in the last 20 years have shown a benefit of postoperative chemotherapy and postoperative chemotherapy combined with radiation (GITSG, EORTC and subsequent analyses). Standard treatments currently based on an international consensus include surgery, radiotherapy and chemotherapy as inseparable modalities.
A comparative dosimetric study of proton and photon radiotherapy of the pancreatic beds and the draining lymph areas shows a clear advantage of protons. The reduction of the dose to the liver, kidneys, small intestine, stomach and spinal cord is statistically significant. In proton radiotherapy, the total dose may be increased and administered even in larger fractions. The total irradiation time is up to 50% shorter.
Experience with Proton Therapy
Radiotherapy with heavy particles, mostly protons, was practically verified in several centres in the US and Japan. Other departments dealt with dose distribution modelling. Published studies include dozens of treated patients. The results can be summarized in the following way:
Postoperative radiation after resection of the pancreas is used to reduce the risk of recurrence of the disease. The target volume includes the pancreatic bed and the draining lymph area. The methodology for determining the lymph areas at risk was published. The therapeutic margin in postoperative radiotherapy of pancreatic carcinoma is minimal owing to the anatomic arrangement of subhepatic structures and the complex lymphatic drainage in the area.
Standard techniques of photon radiation (3D-CRT, IMRT) are associated with a high risk of adverse effects. Acute adverse effects include, in particular, gastrointestinal complications, acute radiation gastritis and enteritis. Adverse effects are common also with respect to the haematopoetic system – leukopenia, thrombocytopenia and after some time anaemia. Chronic adverse effects are based on radiation damage of the liver, kidneys and possibly hollow organs – the stomach and intestines. The statistics of late adverse effects are not complete due to the short survival time of the patients. In addition, radiation doses in the described cohorts do not exceed 50-56 Gy and “dose constraints” are consistently adhered to, reducing the risk.
A technique of postoperative irradiation of the pancreatic bed and of the draining lymph tract has been developed in PTC Prague. The irradiated volume is determined using the RTOG standards. The Pencil Beam Scanning (PBS) technology has very favorable dosimetric parameters, which are the basis for reducing toxicity.
Postoperative irradiation can be administered in 20 to 25 fractions, with the dose of 2.0–2.5 CGE per fraction. Postoperative irradiation is always combined with chemotherapy. It is administered in the form of tablets (capecitabine) or an infusion (gemcitabine) during the irradiation therapy. Postoperative irradiation is followed by standard adjuvant chemotherapy. An important principle must be adhered to in postoperative irradiation of the pancreas: Irradiation is not a substitute for postoperative chemotherapy administered at specialised clinical oncology sites. Both modalities are significant, complement one another and enhance the efficacy of treatment. PTC Prague cooperates with respective surgeons and oncologists to ensure the continuity of all complementary methodologies.
Figure 1: Example of an irradiation plan and dose distribution to individual organs – as can be seen from the dose distribution, a significantly smaller amount of healthy tissue is irradiated with proton therapy.
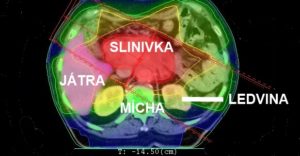
Photon plan
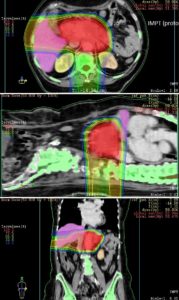
Proton plan
Table 1: Doses to individual structures/organs
| IMRT (photons) | IMPT (protons) | |
| Target volume (pancreatic cancer) | 50 Gy (100%) | 50 Gy (100%) |
| Liver (Dmean) | 33 Gy (66%) | 16 Gy (32%) |
| Right kidney (Dmean) | 12.8 Gy (25.6%) | 3.4 Gy (6,8%) |
| Left kidney (Dmean) | 9.6 Gy (19.2%) | 7.5 Gy (15%) |
Purchase the book via the link below.
Purchase the book via the link below.