 Preparation for Radiotherapy
Preparation for RadiotherapyRadiotherapy is a demanding process and careful preparation of the procedure is required. Ensuring the reproducibility of the same position of the patient and thus the target volume which will be irradiated is absolutely essential. In order to prevent unwanted movements in connection with breathing, at PTC we use the controlled breathing technique, also known as Deep Inspiration Breath Hold (DIBH). Breathing movements are monitored using the Dyn’R device, which measures the amount of inhaled and exhaled air. The system consists of a spirometer, mouthpiece, nose clip (against air passage through other ways than the mouth into the spirometer) and glasses transmitting breath cycle images to the patient and helping them to regulate deep breath-hold to individually pre-set limit.
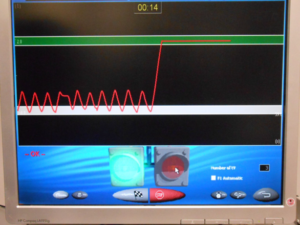
At the beginning of the planning process, the patient is invited to practice controlled breathing. During this process, we determine the depth of the retained breath (the “green band” of the visualized scale). Planning CT, simulation (verification, control) of the irradiation plan, as well as the actual irradiation, are performed by the Dyn’R system. The internal target volume (ITV) is determined on the basis of movement. After breathing training and planning CT execution, the irradiation plan is prepared within a few working days. The proton radiation plan for breast cancer is very simple and often has one or two direct fields. After creating and simulating the irradiation plan, the patient is invited for treatment. Irradiation is performed in the supine position, using the above-mentioned technique. Breathing information and instructions for inhalation and exhalation are displayed to the patient via special glasses. The display is graphically simple and clear, but requires the active cooperation of the patient.
Before each irradiation, the patient is carefully placed in the same position. Precision is absolutely essential for the perfect execution of the treatment, therefore great emphasis is placed on it. The patient’s setup takes longer than the irradiation itself. When adjusting the patient, two X-rays are taken, according to which the correct position of the patient is checked. In this step, the staff checks the adjacent bone structures, the position of the shoulder joint and the contrast clips in the breast (in patients after partial surgery). The possible deviation is up to 5 mm (Picture 3).
In addition, the correct position of the patient and thus the irradiated area is checked by means of two infrared stereoscopic cameras in the irradiation room. These cameras monitor the patient’s body surface and check the correctness of their position (Vision RT). Infrared stereo cameras capture the patient’s body surface and the scanned surface is compared to a virtual body surface that is exported directly from the planning system. From the difference, the correction vector (three translations and three rotations) is calculated and the accuracy of the setting is evaluated (Picture 4). Body surface monitoring is a completely independent check of the correctness of the settings.
After precise adjustment of the patient, irradiation takes place in the DIBH. The proton beam is triggered if the patient is at the correct respiratory level (in the “green band” of the visualized scale). The patient needs to maintain the breath at this level for at least 20 seconds. If the patient exhales, irradiation is automatically interrupted. Several 20 second breaths are required for one fraction (irradiation session).
Individual treatment doses are given each day, Monday to Friday. The total irradiation time is 4-6 weeks.


Purchase the book via the link below.
Purchase the book via the link below.