
The target volume is breast after partial mastectomy or chest wall after total mastectomy. Irradiation of the descending nodes represents the axillary nodes (stage I., II., III.), the supra-key, sub-key nodes and the internal mammary nodes.
With protons, the breast is irradiated with two tangential fields. When using some modern multi-field techniques, such as intensity modulated radiotherapy (IMRT), the volume of irradiated tissue may increase. This 3D conformal radiotherapy can lead to the application of high doses to surrounding healthy organs (heart, coronary arteries, lungs and contralateral breast). In contrast, proton radiotherapy allows the choice of simple irradiation techniques with a small number of irradiation fields, leading to a much lower integral dose. At the same time, it is possible to comply with the limit doses to critical organs (healthy organs close to the target volume), even when the dose escalates to the target volume.
With unnecessary exposure of healthy tissues to radiation, cardiotoxicity, pneumotoxicity or the formation of secondary tumors (tumors induced by radiation) may develop over time.
As respiratory movements may impair the correct and precise execution of proton irradiation, in the treatment of breast cancer we use the method of controlled breathing (picture 1). This way, the target volume (breast/chest wall or the descending nodes) usually does not change during irradiation. There are several situations where the irradiation volume may change before or during irradiation. An example is postoperative seroma or hematoma, which may progress or regress. If the patient has seroma in the irradiated breast, it should be checked regularly via CT, usually once a week. The finding is evaluated with the initial planning CT. In case of unacceptable changes, it is necessary to replan the irradiation volume. A similar situation occurs in the case of progression of edema of the irradiated area with the need for replanning. Another example is a change in the patient’s weight, usually after previous chemotherapy – the difference can only be -/+ 2 kg. The change is recognized when the patient’s body surface is detected using two stereoscopic cameras. Even in this case, replanning is necessary, as this could lead to underdosing of the target volume or undesired increase of the dose to the surrounding healthy tissues.
Acute dermal toxicity of higher grades is a relatively frequently reported parameter in proton studies. Due to the absence of a build-up effect in proton radiotherapy, it is necessary to include the skin as a critical organ in the planning process and thus optimize the dose in the planning process. We also draw the skin at our workplace, it is usually a structure 5 mm below the surface of the target planning volume. By optimizing the dose to the skin as an organ, higher-grade acute toxicity is avoided, which could lead to unwanted post-radiation fibrosis over time.
Proton radiotherapy for breast cancer is a very accurate but technically demanding method. It requires not only careful planning, but also precise daily execution.
For this reason, it is necessary to perform control CT scans during therapy and to monitor positional and volume changes in the area of the irradiated volume compared to the planning CT scan. In case of significant changes, it is necessary to proceed with replanning. The dermal toxicity described in some previous studies is due to the use of the older passive scattering technique. Pencil beam scanning (PBS) allows for significantly better surface dose reduction, and body surface dose can be reduced during planning. It should be borne in mind that for three-dimensional conformal radiation therapy (3D CRT), the surface area is always underdosed due to the “built-up” effect, and this underdosing should also be copied for proton radiotherapy if the cosmetic results are to be comparable or better. This is the only way to ensure accurate and gentle irradiation for patients with breast cancer.

Controlled breathing technique
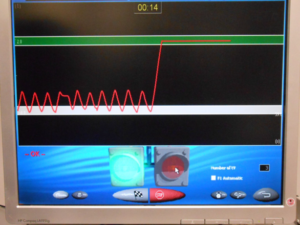
Respiratory curve displayed at deep breath-hold
Purchase the book via the link below.
Purchase the book via the link below.