One of the options for improving the therapeutic profile of treatment for locally and locoregionally advanced malignant tumors of the head and neck is using another type of radiotherapy with a more suitable dose distribution profile. This option is proton radiotherapy. Proton radiotherapy makes it possible to reduce the risks of RT for healthy tissue and to increase the likelihood of curing the tumor due to the possible increase of the overall dose to the tumor region.
The main advantage of proton therapy derived from the Bragg peak allows to deliver a predefined dose with high accuracy anywhere in the body directly into the tumor. Healthy tissue lying in front of tumors (approximately 30% of the absorbed energy protons) is preserved and complete protection of healthy tissue behind the tumor, because it does not absorb any energy. It also allows you to increase the dose to the tumor target volume, increasing thereby the likelihood of local disease control. At a given dose, unwanted side effects on healthy tissue are reduced.
Figure 1 and Table 1 show an example of an irradiation photon IMRT and proton IMPT plan and dose distribution to individual organs. It is clear that a significantly lower or zero dose is applied to healthy tissue with proton radiotherapy.
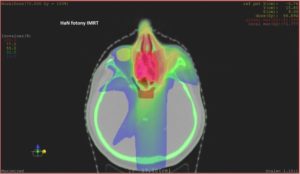
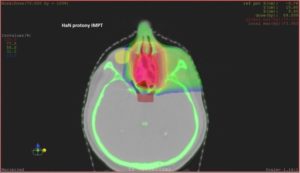
Table 1: Doses to individual structures/organs
| IMRT (photons) | IMPT (protons) | |
| Target volume (ethmoidal cavity) | 70 Gy (100%) | 70 Gy (100%) |
| Eyes (lens) Dmax | 10,11 Gy (14,3%) | 1,77 Gy (2,5%) |
| Brain stem Dmax | 28,6 Gy (40,8%) | 0,47 Gy (0,6%) |
| Chiasma opticumDmax | 46,9 Gy (67%) | 44,1 Gy (63%) |
| Chiasma opticum Dmean | 31,5 Gy (45%) | 5,0 Gy (7%) |
When comparing conventional and proton RT, there is a clear benefit in reducing the burden on the healthy tissues and increasing the dose delivered to the tumor. This dose reduction is not limited to a single organ. On the contrary, it is a complete reduction of radiation exposure to healthy tissues. The level of this reduction is individual. For example, the dose used to irradiate the brain tissue in patients with tumors of the nasopharynx or paranasal sinuses is usually reduced to 10-20% of the usual dose for intensity-modulate photon radiotherapy (IMRT). The dose reduction to the swallowing path and larynx is usually about 50% for the above diagnoses during irradiation of the bilateral cervical lymph nodes.
In properly selected indications, proton radiotherapy allows the administration of high doses of radiation in combination with chemotherapy, with minimal risk of hospitalization, percutaneous endoscopic gastrostomy and treatment with opioid analgesics.
Purchase the book via the link below.
Purchase the book via the link below.